Cancers, Vol. 12, Pages 921: The Glasgow Prognostic Score at Diagnosis Is a Predictor of Clinical Outcome in Patients with Multiple Myeloma Undergoing Autologous Haematopoietic Stem Cell Transplantation
Cancers doi: 10.3390/cancers12040921
Authors:
Hanno M. Witte
Bastian Bonorden
Armin Riecke
Harald Biersack
Konrad Steinestel
Hartmut Merz
Alfred C. Feller
Veronica Bernard
Sebastian Fetscher
Nikolas von Bubnoff
Niklas Gebauer
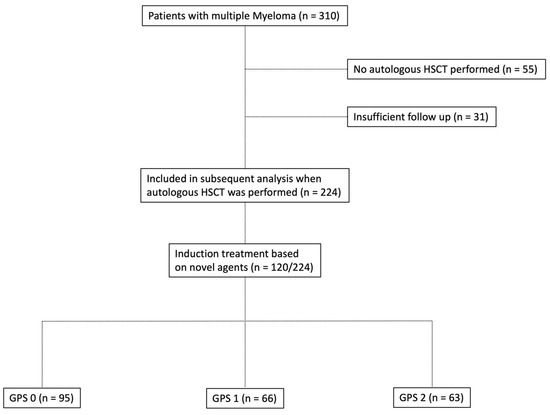
Background: Immunity and inflammatory response affect the tumour microenvironment and the progression of malignancies. Metabolic and inflammatory parameters and ratios of the peripheral blood correlate with outcome in cancer patients. There exist several established and validated inflammation-based scores of prognostic significances including the Glasgow Prognostic Score (GPS). Methods: In this retrospective, multicentre study, we investigated the prognostic capabilities of baseline GPS in patients with multiple myeloma (MM) undergoing autologous stem cell transplantation as a complementary resource for risk stratification. For GPS calculation, a C-reactive-protein (CRP) value of >10 mg/dL counts as one point and an albumin value of <35 g/L connotes another point, resulting in three different subgroups (group I: 0 points; group II: 1 point; and group III: 2 points). Patients with MM admitted to the participating institutions between January 2010 and July 2018 were screened, and established prognostic scores and ratios were assessed. Characteristics significantly associated with overall survival (OS) or progression-free survival (PFS), upon univariate analysis, were included in a Cox proportional hazards model. Results: Following initial assessment, we identified 224 fully evaluable patients who underwent autologous haematopoietic stem cell transplantation for multiple myeloma. A centralised review of pathology and cytogenetic reports was conducted, and a central hematopathology assessment was performed in 175 of 224 cases (78.1%). Proceeding to high-dose chemotherapy and subsequent autologous stem cell transplantation was the main inclusion criterion for all transplant-eligible patients in the study. The median age at diagnosis was 59 years (range: 35–76 years) with a median follow-up of 76 months. Multivariate analysis revealed neutrophil–platelet score (NPS) (HR = 0.528, 95% CI = 0.284–0.984) and B symptoms at primary diagnosis (HR = 1.838, 95% CI = 1.232–2.740) to be independent predictors of PFS while high-risk cytogenetic changes (HR = 2.358, 95% CI = 1.413–3.934, p = 0.001) could be identified as an independent predictor of OS, and GPS to be the only independent predictor of both OS and PFS (OS: HR = 2.127, 95% CI = 1.431–3.162, p < 0.0001 and PFS: HR = 1.405; 95% CI = 1.058–1.867, p = 0.019). Conclusions: Our data show that baseline GPS correlates with rates of relapse and refractory disease in MM patients undergoing autologous transplantation. In a multivariate analysis, these effects were proven to hold prognostic capabilities beyond and independent from established prognosticators. These results require further validation in a prospective setting.

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου